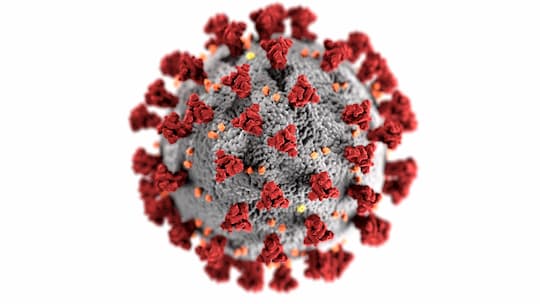
A model of SARS-CoV-2 infection suggests the virus will become as mild as a common cold across the years.
The COVID-19 pandemic is having a devastating impact on people’s physical and mental health, the economy, children’s education, and much more across the world, but would be there an ‘endgame’ for the virus.
According to a model developed by scientists from Emory and Penn State, the virus will become endemic as seen in other known human coronaviruses and so it will become a very low-level threat, like a common cold.
The model uses SARS-CoV-1 and the four coronaviruses responsible for more than a quarter of all common colds.
SARS-CoV-2 is very similar to the SARS-CoV-1 virus but it has ten times the binding affinity to human cell receptors compared to SARS-CoV-1.
Dr Jennie Lavine, the study’s first author, noted that the phrase ‘herd immunity’ for those viruses is partial and somewhat misleading.
The four common cold coronaviruses have long been known since most people are infected during their childhood.
Infection in general makes children develop natural immunity which protect them against severe illnesses in later life but it doesn’t mean that it can stop the recurrence of reinfection.
Dr Lavine said:
“Reinfection is possible within one year, but even if it occurs, symptoms are mild and the virus is cleared from the body more quickly.
It highlights the need to tease apart the components of immunity to SARS-CoV-2.
How long does immunity that prevents pathology last, and how long does immunity that prevents transmission last?
Those durations may be very different.”
Recent papers on lasting immunity and antibodies against COVID-19 in recovered patients are continuously providing reliable data, however, the part regarding protection or blocking of transmission remains a puzzle.
Dr Lavine said:
“Overall, we’re asking: how does SARS-CoV-2 compare to other viruses such as seasonal influenza or respiratory syncytial virus.
This model assumes immunity to SARS-CoV-2 works similar to other human coronaviruses.
We don’t really know what it would be like if someone got one of the other coronaviruses for the first time as an adult, rather than as a child.”
Once COVID-19 becomes endemic, the model foresees the infection fatality ratio (percentage of deaths amongst infected patients) could drop below seasonal influenza (a rate of 0.1%).
Professor Ottar Bjornstad, study co-author, said:
“We are in uncharted territory, but a key take-home message from the study is that immunological indicators suggest that fatality rates and the critical need for broad-scale vaccination may wane in the near term, so maximum effort should be on weathering this virgin pandemic en route to endemicity.”
The authors hint that a COVID-19 vaccination can save hundreds of thousands people during the first or second year of vaccine rollout.
However, ongoing mass vaccination may be unnecessary when SARS-CoV-2 becomes endemic, except for those who are in vulnerable groups.
They add that SARS-CoV-2 infection rates in infants and young children appear to be mild with low mortality.
If children experience severe SARS-CoV-2 infection, like MERS-CoV (Middle East respiratory syndrome-related coronavirus), then routine vaccinations will become critical.
The study was published in Science (Lavine et al., 2020).