Brain shrinkage was six times more likely in those with low levels of this vitamin.
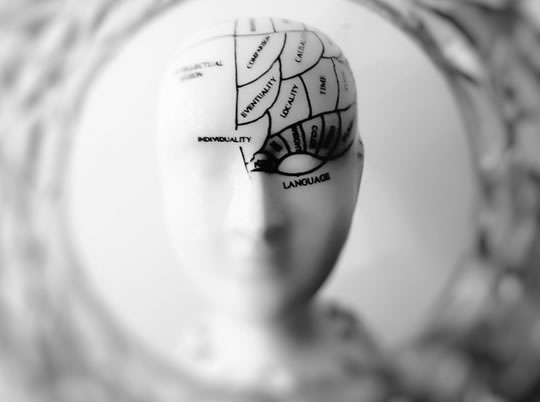
Vitamin B12 may protect against brain shrinkage with age, research finds.
People with higher vitamin B12 levels were six times less likely to suffer brain shrinkage.
Vitamin B12 levels can be boosted through supplementation or by eating foods such as dairy, liver, salmon and eggs.
Fortified breakfast cereals also contain vitamin B12.
Around one-in-four people may have a vitamin B12 deficiency — however none of the people in the study were deficient.
People who may have difficult getting enough vitamin B12 include vegetarians, older people and those with some digestive disorders, such as Crohn’s disease.
The study included 107 older people who had brain scans, memory testing and their blood levels were checked for vitamin B12 levels.
Dr Anna Vogiatzoglou, the study’s first author, said:
“Many factors that affect brain health are thought to be out of our control, but this study suggests that simply adjusting our diets to consume more vitamin B12 through eating meat, fish, fortified cereals or milk may be something we can easily adjust to prevent brain shrinkage and so perhaps save our memory.
Research shows that vitamin B12 deficiency is a public health problem, especially among the elderly, so more vitamin B12 intake could help reverse this problem.
Without carrying out a clinical trial, we acknowledge that it is still not known whether B12 supplementation would actually make a difference in elderly persons at risk for brain shrinkage.”
Vitamin B12 is involved in the production of red blood cells.
A deficiency — which is more frequent in those over 60 — can cause anemia, which is a lack of red blood cells.
Dr Vogiatzoglou continued:
“Previous research on the vitamin has had mixed results and few studies have been done specifically with brain scans in elderly populations.
We tested for vitamin B12 levels in a unique, more accurate way by looking at two certain markers for it in the blood.”
The study was published in the journal Neurology (Vogiatzoglou, et al., 2008).