Alzheimer’s causes degeneration in part of the brain that controls this function first.
Alzheimer’s causes degeneration in part of the brain that controls this function first.
Excessive napping during the day can be an early sign of Alzheimer’s, the most common form of dementia.
Scientist tended to assume that people with Alzheimer’s disease are drowsy during the day because of poor sleep at night.
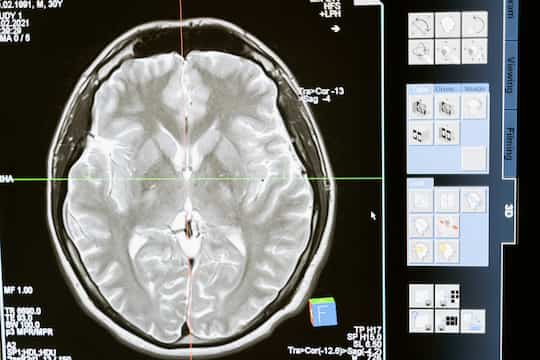
Research has now shown, though, that it is due to the degeneration of neurons that maintain wakefulness.
The tau protein, one of two proteins involved in Alzheimer’s, is responsible for the critical neurodegeneration.
Alzheimer’s causes degeneration in this part of the brain first, which is why daytime napping without night time sleep problems is an early sign of dementia.
Professor Lea T. Grinberg, study co-author, said:
“We were able to prove what our previous research had been pointing to—that in Alzheimer’s patients who need to nap all the time, the disease has damaged the neurons that keep them awake.
It’s not that these patients are tired during the day because they didn’t sleep at night.
It’s that the system in their brain that would keep them awake is gone.”
Many of the key neurons are in the hypothalamus, a part of the brain that is central for wakefulness and arousal.
These neurons are so important as they affect a large number of other critical nerve cells.
Mr Joseph Oh, the study’s first author, explained:
“You can think of this system as a switch with wake-promoting neurons and sleep-promoting neurons, each tied to neurons controlling circadian rhythms.
It’s a small number of neurons but their computational capabilities are incredible.
When these cells are affected by disease, it can have a huge effect on sleep.”
The conclusions come from a study of 33 patients with Alzheimer’s that were compared to normal controls.
Dementia and sleep
Many other studies have found a link between dementia and sleep.
People who sleep for too little or too long are at a higher risk of cognitive decline and dementia.
Indeed, people who sleep more than 9 hours a night have double the risk of developing dementia, one study found.
However, those who sleep for between 5.5 and 7.5 hours per night do not see declines in their cognitive health, even when suffering the early effects of Alzheimer’s disease.
Those sleeping longer also have lower brain volumes.
Also, getting less REM sleep — the phase in which we dream — is linked to dementia.
During sleep the brain cycles between periods of deep sleep and then up towards shallower periods of sleep in which we tend to dream, whether we remember those dreams or not.
During REM sleep the eyes move rapidly from side-to-side (hence Rapid Eye Movement Sleep).
The study was published in JAMA Neurology (Oh et al., 2022).